Chief Corner: Aspiration Pneumonitis vs. Aspiration Pneumonia
/Background:
Aspiration is a common occurrence both inside and outside of the hospital. Internal medicine physicians need to be able to differentiate between aspiration pneumonitis and aspiration pneumonia since treatments for each differ. The need for anaerobic coverage in aspiration pneumonia is often a common question on the wards as well. In this post we’ll discuss the two diagnoses, ways to differentiate between the two, and their respective treatments.
Aspiration Pneumonitis vs. Aspiration Pneumonia:
To begin, the most important thing is to define what each entity is. Aspiration pneumonitis is a chemical injury to the lung resulting in an inflammatory response due to aspiration of sterile gastric contents. Aspiration pneumonia is an infection in the lung caused by inhalation of oropharyngeal secretions containing pathogenic bacteria.
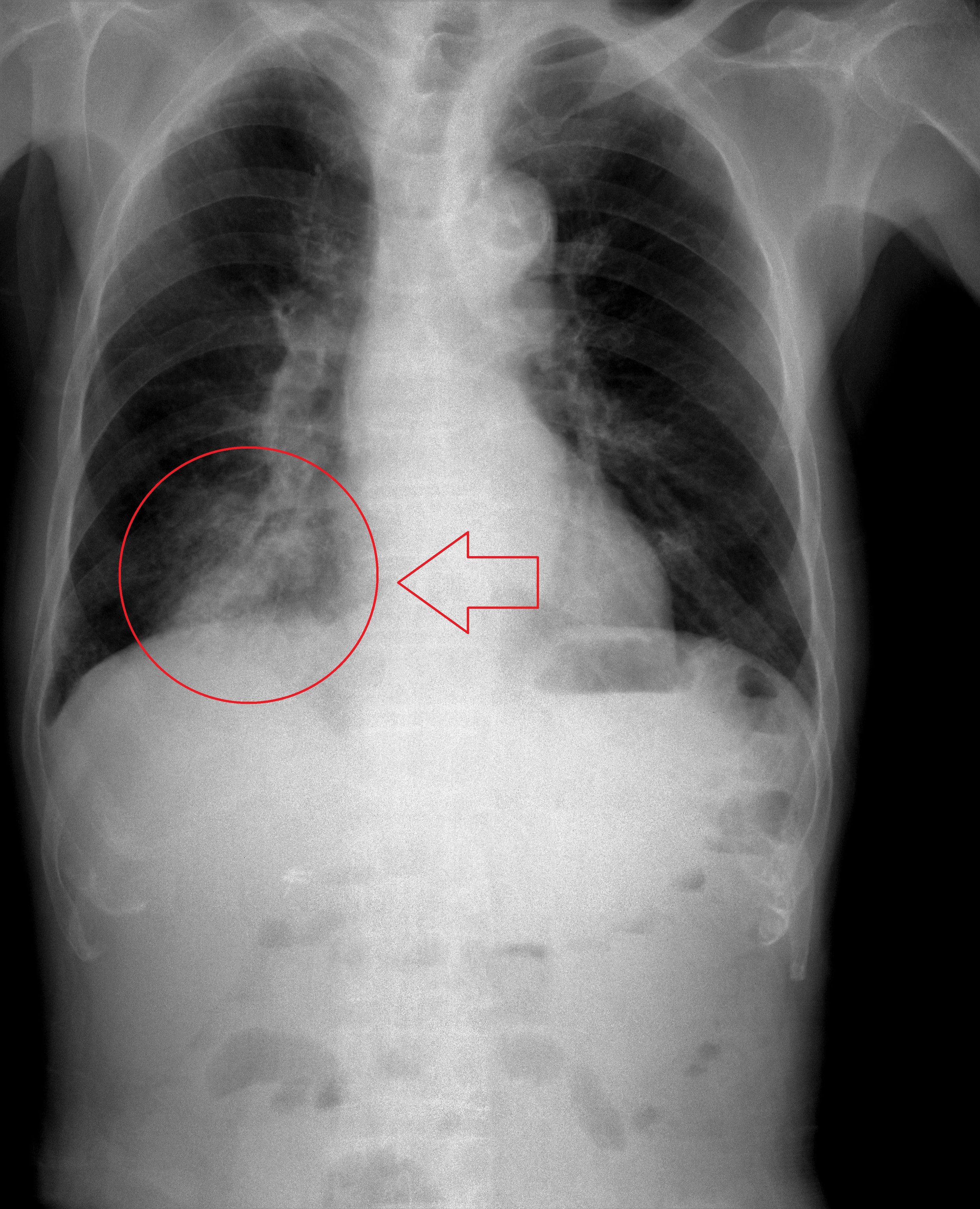
While there is no definitive diagnostic tool to differentiate the two, several clinical characteristics can help distinguish the two diagnoses. Due to the volume of aspiration needed to cause a pneumonitis, aspiration pneumonitis typically occurs after a witnessed aspiration event. In addition, aspiration pneumonitis is a hyperacute process resulting in immediate acute respiratory distress and hypoxia typically within hours of aspiration. This is due to direct caustic effects of the acidic gastric contents followed by neutrophil infiltration into the alveoli. Symptoms often resolve within 48 hours. Aspiration pneumonia on the other hand is more likely with unwitnessed aspiration events and symptoms may not occur for up to 48 hours after the event. Like all other pneumonias, aspiration pneumonia is a clinical diagnosis with suggestive features including fever, dyspnea, and chest X-ray consolidation. Aspiration pneumonias tends to occur in dependent areas of the lung including the posterior segments of the upper lobes and superior segments of the lower lobes, especially on the right side. Unfortunately studies looking at biomarkers including procalcitonin have failed to reliably distinguish the pneumonitis from pneumonia.
Treatment for aspiration pneumonitis and pneumonia differ as well. Aspiration pneumonitis requires largely supportive therapy including oxygen, airway clearance, and bronchodilators if necessary. In general, steroids are not recommended. Antibiotics should not be given for aspiration pneumonitis unless symptoms persist for greater than 48 hours or if the patient has a condition resulting in bacterial colonization of gastric contents such as a small bowel obstruction. Aspiration pneumonia has been thought to be classically an anaerobic infection however newer studies suggest a more polymicrobial infection with a minority being anaerobes. Antibiotics are essential and choice should be based on the patient’s history, exposure to hospital-acquired pathogens, and local resistance patterns. The inclusion of anaerobic coverage should not be routine. Instead anaerobic coverage is likely only warranted in patients with severe periodontal disease, putrid sputum, or in cases of necrotizing pneumonia or lung abscess.
Learning Points:
- Aspiration pneumonitis and pneumonia can often be clinically differentiated based off the nature of the aspiration event, time course of symptoms, and clinical features including chest X-ray findings
- Aspiration pneumonitis tends to be a hyperacute process in which symptoms resolve within 48 hours with supportive care
- Aspiration pneumonia is often a polymicrobial infection and may not include anaerobes as once classically thought
- Antibiotics choice for aspiration pneumonia depends on several patient characteristics but should routinely include activity against gram-negative organisms
- Patients with aspiration pneumonia with severe periodontal disease, putrid sputum, necrotizing pneumonia, or lung abscess warrant antibiotics with anaerobic coverage. Those without the above features likely do not
References:
- Marik, P. "Aspiration Pneumonitis and Aspiration Pneumonia." New England Journal of Medicine, vol. 344, no. 9, 1 Mar 2001, pp.665-71.
- DiBardino, DM et al. "Aspiration pneumonia: a review of modern trends." J Crit Care, vol. 30, no. 1, Feb 2015, pp. 40-48.
- <https://commons.wikimedia.org/wiki/File:Aspiration_pneumonia201711-3264.jpg>
Authored by: GREGORY WIGGER, MD