I Got a Fever, and the Only Prescription is More Blood Cultures?
/I occasionally moonlight at a local rehabilitation facility. One night recently I was called by a nurse because a patient had spiked a fever to 102.4°. She asked what I wanted to do. I reflexive went to order blood cultures and then thought, “Does this patient need this?” He was hemodynamically stable with minimal complaints. He had recently been discharged from an outside hospital after getting treatment for a UTI. I ordered the blood cultures, which grew Klebsiella the following day. I couldn’t help feeling that I’d got lucky. Calls on nights or cross-cover shifts are so often about a patient’s fever. The “culture if spikes” dogma has permeated training such that we order blood cultures without even stopping to think about it. So I read up on bit on blood cultures in the setting of a fever.
First of all, why is there any concern with ordering blood cultures? Well it comes down to two things: 1) the potential risks with cultures, and 2) the diagnostic use of blood cultures in the setting of a fever. The risk lies in false positive cultures which lead to repeat blood cultures, further diagnostic studies, and unnecessary antibiotic use. These in turn lead to increased hospital cost and length of stay [1].
So what is the yield of blood cultures in febrile patients? Unfortunately, there are no agreed upon guidelines for this question. One study looking at over 550 blood cultures in more than 300 patients found the true positive rate of only 3.6% per order [2]. The most common indication for ordering blood cultures was fever and fever + additional indications (i.e. leukocytosis, rigors, etc.) The primary diagnoses most predictive of a true positive culture were unsurprisingly bacteremia and endocarditis. The clinical characteristic most predictive of true positive blood culture was the absence of recent antibiotics [2].
What about patients that are admitted for a suspected infection, started on antibiotics, and continue to have fevers? A retrospective study looked at the yield of blood cultures in 139 patients admitted for infection and started on antibiotics. Only one blood culture (0.72%) in the review isolated a new pathogen compared to pre-antibiotic cultures [3]. This and other data suggests that repeat cultures should not be collected during the first 72 hours of antibiotics, even with fever, given that they rarely isolate new pathogens from pre-antibiotic blood cultures [3].
Often you will hear of the importance of blood culture timing with fever, perhaps it plays a role in the low true positive rates. However studies have shown that the timing of cultures in relation to the fever doesn’t seem to matter for yield [1, 4]. The blood volume collected is the most critical variable for blood cultures. The IDSA recommends 20-30 cc per culture [4].
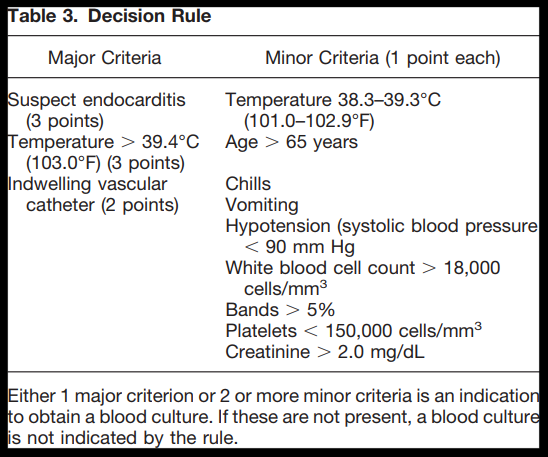
Several clinical decision aids have been created to guide physicians in the decision to culture as shown below [6]. It’s important to note that many of these decision aids are created for patients in the emergency room patients, instead of admitted patients, and are based on retrospective data. Thus they are largely recommended as a starting point in the decision rather than final determination [7].
With all this information, we return to the original question – in patients with a fever, who should have blood cultures collected? Well like most things in medicine, it’s a clinical decision. Fever alone is NOT an indication to get blood cultures. So go ahead and forget the “culture if spikes” dogma. Instead the decision to order blood cultures should depend on multiple things including your clinical suspicion for bacteremia, supporting clinical signs and symptoms, and the patient’s history. Suspicion for diagnoses like endocarditis should prompt further consideration for cultures. Certain populations including the elderly and immunosuppressed should lower the threshold to culture given their impaired ability to mount a febrile response [1]. In addition, if a patient is admitted for a suspected infection and started on antibiotics, repeat blood cultures are not necessary for fevers that occur within the first 72 hours of treatment unless there is a significant change in clinical status.
Going back to my patient that I was called for overnight. His admission labs showed a worsening leukocytosis compared to days prior, he had history of a recent infection, and, with probing, his nurse indicated that she had noticed a change in the color and smell of his urine. Thus, clinical suspicion for infection was increased and he warranted getting blood cultures with a fever.
So next time you’re on long call or overnight and you get that call about a patient having a fever, think:
Are there any other signs or history to suggest infection/bacteremia?
Is this patient on antibiotics? Have they been on for less than 72 hours?
Am I suspecting a diagnosis with a high likelihood for bacteremia like endocarditis?
Maybe I just need more cowbell?
References
Chestnutt, B et al. “Blood cultures for febrile patients in the acute care setting: Too quick on the draw?” Journal of the American Academy of Nurse Practitioners. Vol 20: 539-46. 2008.
Linsenmeyer, K et al. “Culture if Spikes? Indications and Yield of Blood Cultures in Hospitalized Medical Patients.” Journal of Hospital Medicine. Vol 11(5): 336-40. May 2016.
Grace, C et al. “Usefulness of Blood Culture for Hospitalized Patients Who Are Receiving Antibiotic Therapy.” Clinical Infectious Diseases. Vol 32: 1651-55. June 2001.
Riedel, S et al. “Timing of Specimen Collection for Blood Cultures from Febrile Patients with Bacteremia.” Journal of Clinical Microbiology. Vol 46(4): 1381-85. April 2008.
Barron, E et al. “A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2013 Recommendations from IDSA and ASM.” Clinical Infectious Diseases. Vol 57(4): e22-121. August 2013.
Shapiro, N et al. “Who Needs a Blood Culture? A Prospectively Derived And Validated Prediction Rule.” Journal of Emergency Medicine. Vol 35(5): 255-64. 2008.
Bair, A et al. “Who Needs a Blood Culture in the ED?” NEJM Journal Watch. November 2008.
Authored by: GREGORY WIGGER, MD