Distance Learning: Chemotherapy Side Effects
Objectives
Discuss the presentation and timing of chemotherapy, immunotherapy, and small molecular therapy side effects
Review the common chemotherapy related side effects and their management
Apply to presentations of these effects in the outpatient and inpatient setting
Theory
Additional Resources
Cases
Case 1: You are evaluating Mr. Watts in the clinic because his wife thinks she must raise her voice more to get his attention for the last couple of weeks and he has been leaving the volume on the TV up at home. He is a 53 year old male with a history of a germ cell tumor of the left testicle s/p removal after PET scan was negative for metastasis. Four months ago, he was started on adjuvant chemotherapy (cisplatin and etoposide with dexamethasone). He takes no other home medications.
Discuss your evaluation of this patient and how you approach hearing loss?
Case 2: You are evaluating a 49 y/o F with PMH of HTN, DMII and stage III adenocarcinoma of the right lung in the the ED 5 days after her first infusion of chemotherapy. She reports that after the infusion she had some minor nausea the day of but felt well until yesterday when she developed a headache, muscle aches, and extreme malaise. Her chemotherapy is carboplatin, pemetrexed, pembrolizumab.
Temperature: 101.2
Blood Pressure: 100/60
Heart Rate: 92
Respiratory Rate: 21
SpO2: 95% on Room Air
Discuss your impression of this patient, what are your concerns and do they need to be admitted?
Case 3: Ms. Treg, a 37 y/o F with PMH of Stage III colon cancer currently receiving FOLFIRI+ bevacizumab as neoadjuvant chemotherapy presents to your primary care clinic for headaches. They have been going on since about a week after she received chemotherapy the first time. Her vitals are normal, except her blood pressure which is 158/94. You spend a few minutes speaking with her and take it again to be 148/92. You ask her to try taking some Tylenol at home, and take her BP at home for a few days and call back to clinic. Her home BPs are averaging 140s-150s systolic/90s diastolic.
Discuss your impression of this patient, what should you be thinking about as you evaluate their hypertension?
Case 4: Mr. Nod is a 56 y/o M with PMH of CAD, HTN, DMII (well controlled), and Stage IV renal clear cell carcinoma currently on maintenance pembrolizumab and axitinib currently being called up by the emergency room for shortness of breath. He reports that he has been having dyspnea for the last couple weeks which has gotten progressively worse. He denies typical chest pain, denies peripheral edema, denies wheezing. He does have atypical chest pain on the right side which is constant now, and worse with deep inspiration.
Blood Pressure: 105/67
Heart Rate: 100
Respiratory Rate: 24
SpO2: 89%
Discuss your differential for this patient, what are you worried about?
Case 5: Mrs. Soma is a 76 y/o Female with PMH of RA, CAD, and CLL presenting to your clinic because of palpitations. They have been going on for about a week, she says she just feels her heart beating in her chest, does not change with rest or activity, has no accompanying chest pain or shortness of breath. She does have fatigue but is not sure if this is more than normal. She takes hydroxychloroquine for her RA, ASA/statin for CAD, and ibrutinib for CLL.
Blood Pressure: 136/86
Heart Rate: 142
Respiratory Rate: 19
SpO2: 98%
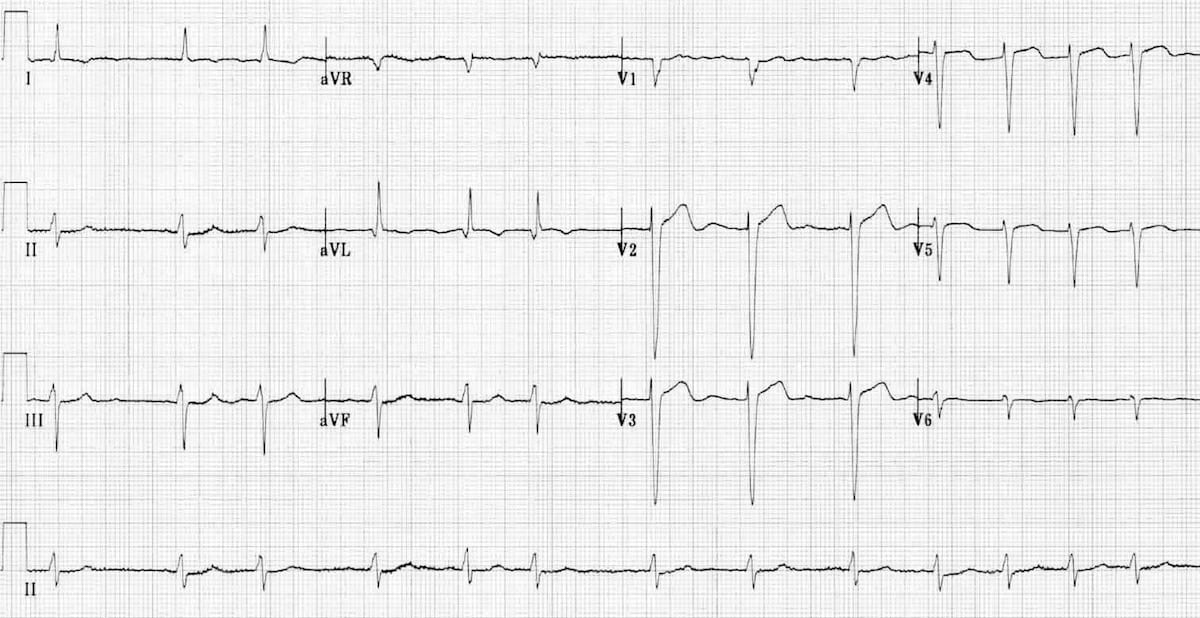
What does the EKG show and how do you approach evaluating this patient?


